The Problem: Guidelines vs. Reality
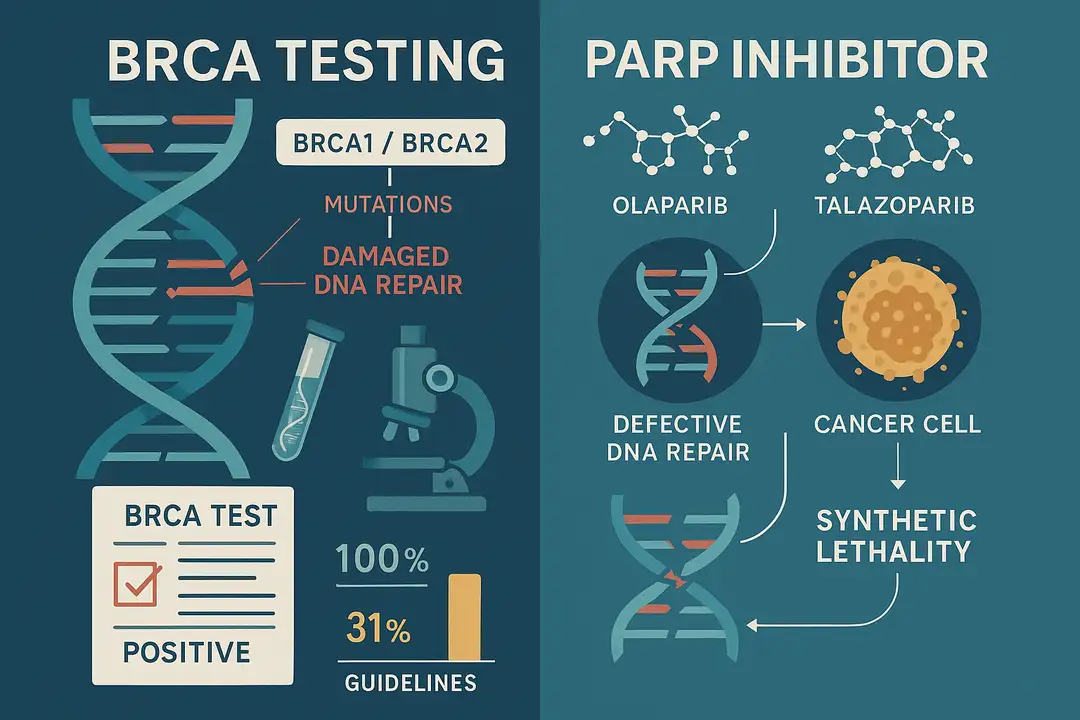
Despite clear clinical guidelines recommending BRCA testing for all patients with HER2-negative metastatic breast cancer, a comprehensive real-world study reveals a troubling gap between recommendations and practice. The analysis of 15,006 patients diagnosed between 2014 and 2022 exposes significant shortcomings in both genetic testing rates and subsequent treatment with PARP inhibitors.
This retrospective study, published in JCO Precision Oncology, utilized data from the US Flatiron Health database to examine real-world patterns of germline BRCA (gBRCA) testing and poly(ADP-ribose) polymerase inhibitor (PARPi) utilization in patients with HER2-negative metastatic breast cancer.
The Numbers: Suboptimal Testing and Treatment
The study's findings reveal stark disparities between guideline recommendations and clinical practice:
Testing Rates: Only 4,654 patients (31.0%) of the total cohort received gBRCA testing during the study period. This means approximately two-thirds of patients with HER2-negative metastatic breast cancer did not receive the genetic testing that current guidelines recommend for all patients in this category.
Mutation Prevalence: Among tested patients, 337 (7.2%) were found to have germline BRCA mutations (gBRCAm), consistent with expected prevalence rates.
Treatment Gaps: From 2018 to 2022, PARPi therapy was initiated in only 94 (45.6%) of 206 patients with gBRCAm. This means more than half of patients with a clear indication for PARPi therapy did not receive it.
Subtype Disparities: Testing rates were consistently lower in patients with hormone receptor-positive (HR+) tumors compared to those with triple-negative breast cancer, despite both groups potentially benefiting from BRCA testing.
Patient Demographics and Temporal Trends
The study included a diverse patient population: 9,561 (63.7%) White, 1,848 (12.3%) Black/African American, 332 (2.2%) Asian, and 19 (0.1%) Hispanic or Latino patients. While gBRCA testing rates increased from 2014 to 2022, the improvement was gradual and insufficient to meet clinical needs.
The persistence of suboptimal testing rates years after the establishment of clear guidelines suggests systemic barriers that extend beyond simple awareness of recommendations.
Clinical Outcomes: The Cost of Missed Opportunities
The real-world survival analysis provides compelling evidence for PARPi therapy's clinical utility. With a median follow-up of 22.8 months, patients with gBRCAm who received PARPi therapy demonstrated numerically longer overall survival compared to those who did not:
- PARPi recipients: 32.3 months (95% CI, 22.7 to 47.4)
- Non-recipients: 21.9 months (95% CI, 18.4 to not reached)
While this difference did not reach statistical significance in the exploratory analysis, the magnitude of the survival difference (approximately 10.4 months) is clinically meaningful and consistent with benefits observed in randomized controlled trials.
Understanding the Barriers
The study identifies several factors contributing to suboptimal testing and treatment patterns:
Complexity of Testing Process: BRCA testing requires coordination between multiple healthcare providers, including oncologists, genetic counselors, and laboratory personnel. Each step represents a potential point of failure.
Access Issues: Many healthcare systems, particularly in rural or underserved areas, lack adequate genetic counseling resources. The shortage of certified genetic counselors has been well-documented.
Financial Considerations: Prior authorization requirements, copayments, and deductibles can create barriers, despite most insurance plans covering BRCA testing for appropriate indications.
Provider Factors: Some oncologists may lack familiarity with genetic testing guidelines or feel uncomfortable interpreting results. Time constraints in busy practices can limit adequate counseling.
Timing Challenges: Testing is often delayed until later lines of therapy, reducing the potential benefit of PARPi therapy when it should ideally inform first-line treatment decisions.
The Economic Impact
The study highlights the economic implications of suboptimal testing patterns. Every patient with gBRCAm who does not receive appropriate testing and subsequent PARPi therapy represents a missed opportunity for improved outcomes. The cost-effectiveness of BRCA testing has been demonstrated in multiple economic analyses, showing that benefits of identifying patients who can benefit from PARPi therapy outweigh testing costs.
Study Limitations and Strengths
The researchers acknowledge several limitations: the retrospective design, potential for unmeasured confounding factors, and the exploratory nature of the survival analysis. However, the study's strengths include its large sample size, diverse patient population, real-world setting, and comprehensive data from electronic health records.
Clinical Implications and Recommendations
The study's findings support several key recommendations:
Systematic Testing Approaches: Healthcare systems should implement systematic approaches to ensure all eligible patients receive timely gBRCA testing, potentially including electronic health record-based alerts and standardized protocols.
Provider Education: Continuing education programs should focus on genetic testing guidelines, practical aspects of test ordering, and results interpretation.
Access Improvement: Healthcare systems should invest in genetic counseling services and consider telemedicine solutions to address access barriers.
Quality Metrics: Current quality measures should be updated to include appropriate genetic testing rates as performance indicators.
Future Directions
The researchers suggest several areas for future investigation: longer-term survival outcomes, cost-effectiveness analyses, and strategies to improve testing implementation. The development of streamlined testing workflows and decision support tools could help address current barriers.
Conclusion: A Call for Systematic Change
This comprehensive real-world analysis reveals a significant gap between the promise of precision medicine and its implementation in clinical practice. The finding that only 31% of patients with HER2-negative metastatic breast cancer received guideline-recommended genetic testing, and less than half of patients with gBRCAm received appropriate targeted therapy, represents a fundamental failure to deliver optimal care.
The survival advantage associated with PARPi therapy can only benefit patients who are identified through appropriate testing and receive timely treatment. Addressing these gaps requires coordinated efforts from healthcare providers, healthcare systems, payers, and patient advocacy organizations.
The study provides compelling evidence for the clinical utility of gBRCA testing and PARPi utilization, while highlighting the urgent need for systematic approaches to improve implementation. The time for incremental improvements has passed—the medical community must commit to ensuring that precision medicine reaches all patients who can benefit from it.
Editorial note: This content was developed with the support of artificial intelligence technologies to optimize the writing and structuring of the information. All material was carefully reviewed, validated, and supplemented by human experts prior to publication, ensuring scientific accuracy and adherence to good editorial practices.
#BRCA #PARPInhibitors #BreastCancer #PrecisionMedicine #RealWorldEvidence
Sources
- Yadav, S., et al. (2025). Real-World Germline BRCA Testing, Poly(ADP-ribose) Polymerase Inhibitor Utilization, and Survival Outcomes in Human Epidermal Growth Factor Receptor 2–Negative Metastatic Breast Cancer. JCO Precision Oncology, 9, e2400814. https://doi.org/10.1200/PO-24-00814.
Highlights
Medical Affairs
Trastuzumab deruxtecan (T-DXd) Provides Significant Clinical Benefit Over Trastuzumab emtansine (T-DM1), Marking a Potential Shift in the Therapeutic Standard for HER2+ Breast Cancer

TribeMD
SnackableHealth™ | From Intervention to Prevention: How Secondary Prevention Clinics Are Redefining Post-ACS Care
Medical Affairs
META-AF: Metformin as an Adjunctive Therapy to Catheter Ablation of Atrial Fibrillation

Medical Affairs
Trastuzumab deruxtecan (T-DXd) Provides Significant Clinical Benefit Over Trastuzumab emtansine (T-DM1), Marking a Potential Shift in the Therapeutic Standard for HER2+ Breast Cancer

TribeMD
SnackableHealth™ | From Intervention to Prevention: How Secondary Prevention Clinics Are Redefining Post-ACS Care
Medical Affairs
META-AF: Metformin as an Adjunctive Therapy to Catheter Ablation of Atrial Fibrillation


